Physiotherapy Neurology Genetic Nerves
Genetic Nerves
Peripheral
Charcot Marie Tooth
Dejerine-Scottas syndrome
Motor
Spinal Muscular Atrophy
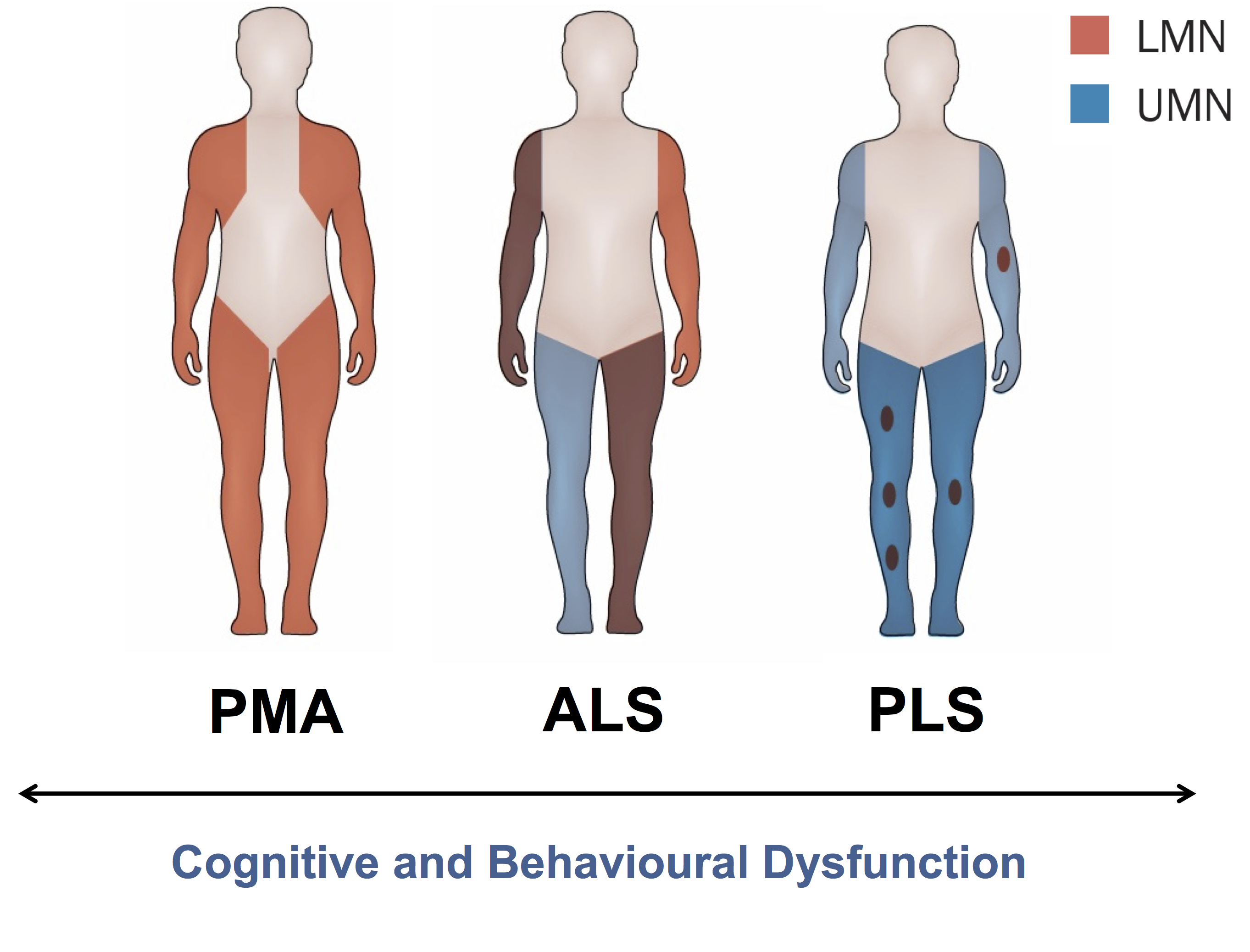
Motor neuron disease
- amyotrophic lateral sclerosis (both UMN and LMN)
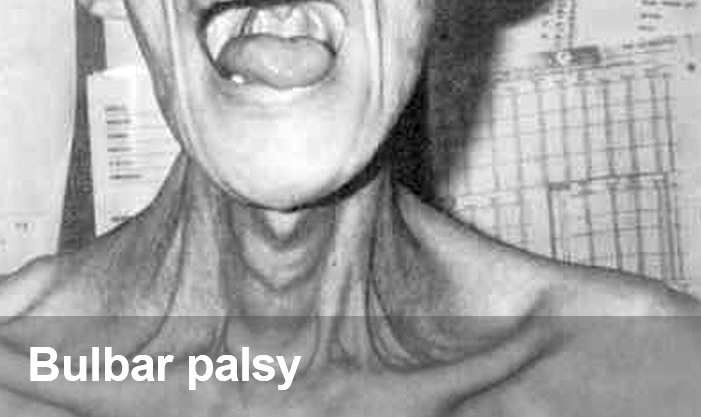
- progressive bulbar palsy (IX glossopharingeal, X vagus, XII hypoglossal)
- progressive muscular atrophy (only LMN)
- primary lateral sclerosis (only UMN)
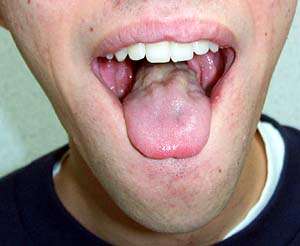
Charcot Marie Tooth
Most common genetic peripheral nerves neuropathy
SSx – loss of sensation and motor function. Onset – childhood to 40 yo. High arch, inverted bottle, feet first

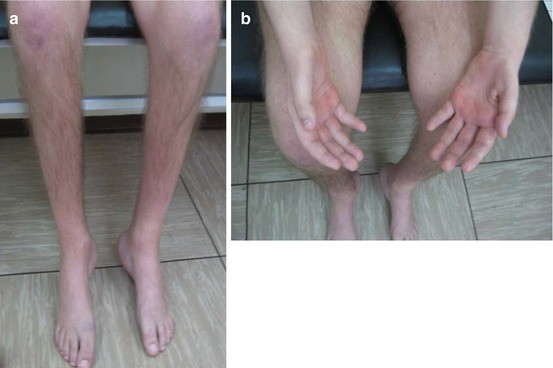

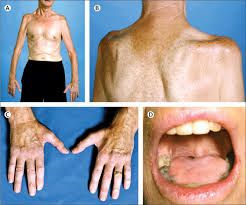
Dejerine-Scottas syndrome
Genetic peripheral nerves neuropathy causing/carachterising/resulting/in which loss of sensation, motor function and muscle waist
Onset – early childhood – extremities
Onset occurs in infancy or early childhood, usually before 3 years of age. Progression is slow until the teenage years at which point it may accelerate, resulting in severe disability.
Symptoms are usually more severe and rapidly progressive than in the other more common Charcot–Marie–Tooth diseases. Some patients may never walk and solely use wheelchairs by the end of their first decade, while others may need only a cane (walking stick) or similar support through life.
Motor
Spinal Muscular Atrophy
SMN1 gene (survival of motor neuron 1)
genetic neuromuscular disorder caused by loss of motor neurons and progressive musles waist
loss of motor neurons prevent signals b/n brain and mm
– infantine type > 2 y o
– intermidiate – juvenile
– adult onset – ptn 30+
SSx – areflexia, mm weakness, decreased mm tone, legs weakness



Motor neuron disease
-
Amyotrophic lateral sclerosis (both UMN and LMN) – Lou Gehrig’s Disease
Disease causes death of neurons controlling voluntary mm
combinating of genetic and environmental factors
SSx mm stiffness and weakness
onset 40-60

-
Primary lateral sclerosis (only UMN)
-


Progressive muscular atrophy (only LMN)


Progressive bulbar palsy (IX glossopharingeal, X vagus, XII hypoglossal)